
Molina
Updated: October 30, 2024
Dignity Health and Molina Healthcare of California
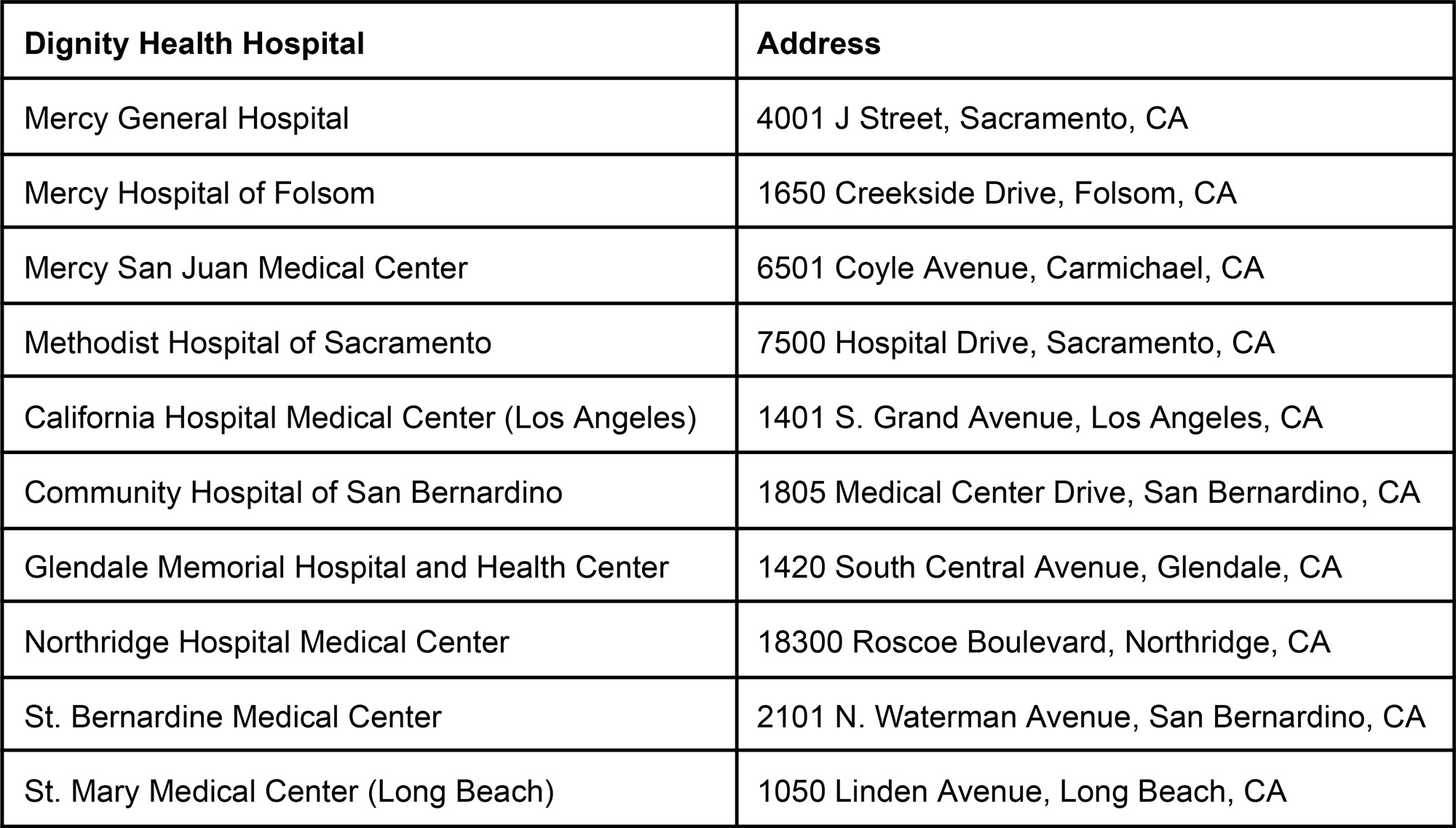
Dignity Health has been working with Molina Healthcare of California (Molina) to renew our contracts. If agreement cannot be reached by December 31, 2024 then the Dignity Health providers listed below will be out of network for Molina members beginning January 1, 2025.
What you need to know:
Don’t delay or cancel your planned care. Nothing will change before January 1, 2025. If you have appointments scheduled at a Dignity Health provider prior to January 1, 2025 you do not need to cancel them.
If our agreements end and you are currently in active treatment with us, you may qualify for Continuity of Care. Continuity of Care is a benefit designed to protect individuals receiving active treatment and intended to protect patients from having to change providers or having care delayed or disrupted if an agreement between a health plan and provider is terminated. This benefit is a state law, and Molina, like all licensed health plans, must abide by the requirements. Healthcare conditions that may be covered by Continuity of Care include:
- Acute conditions needing ongoing treatment such as chemotherapy, hyperbaric treatment, and radiation therapy;
- Chronic conditions including heart disease, diabetes, orthopedic issues and many others;
- Maternity-related care;
- Pediatric care between the ages of birth and 36 months;
- Services related to a terminal illness;
- Authorized surgeries or other procedures scheduled to occur within 180 days of the contract’s termination; or
- Other services previously authorized by Molina.
If you have an emergency, go to the nearest emergency room.
For questions about Continuity of Care eligibility or benefits, please call Molina:
- If you are a Molina Medicare member, call 1-800-665-0898
- If you are a Molina Medi-Cal member, call 1-888-665-4621
- If you are a Molina Marketplace member, call 1-888-858-2150
